|
Table of Content - Volume 20 Issue 3 - December 2021
Tale of a Tailgut cyst: A case report
Isha Vinayak Rokade1, Santosh Dalavi2*, Alka Gosavi3, Prashant Murarkar4
{1JR II, 2Associate Professor, Department of Surgery} {3Associate Professor & HOD, 4Associate Professor Department of Pathology} Government Medical College Miraj, INDIA. Email: isharokade@gmail.com
Abstract Background: Tailgut cyst( TGC) also known as retro rectal cystic hamartoma is a rare congenital pathology that arises -from post-natal primitive gut remnants in the retro rectal-presacral space. Because of the rarity of the lesion and the variability of the anatomical position, its diagnosis and surgical treatment are often difficult. Complete surgical excision of this prevents recurrent draining sinuses and eliminates the possibility of malignant change. Here we describe a unique case in which a tailgut cyst localized in the retrorectal and presacral space presented with pelvic pain and gluteal swelling Keywords: Tail gut cyst, retro rectal cystic hamartoma, teratoma, gluteal swelling
INTRODUCTION TGCs also referred to as retro rectal cystic hamartomas, or postanal gut cysts arise from remnants of the embryonic primitive gut that extends into the transient true tail, which develops between 35 and 56 days of gestation before regression. These lesions are often multicystic and multilocular. Tailgut cysts are more commonly seen in adults. Women are more likely (3:1) to have retro rectal cysts than men.2 They are generally benign, but the malignant transformation has been reported on rare occasions.3-6 Tailgut cysts are almost invariably located in retro rectal or presacral space but have also been reported in various locations such as perirenal space, perineal skin, and, very rarely, pre rectally7,8,3,4 Back or pelvic pain is the most common symptom of a retro rectal tumor, although the clinical presentation is quite variable and can include neurologic symptoms affecting bowel function, bladder function, or constipation, difficulty evacuating, or abdominal pain.2 However, the main problems associated with tailgut cysts are bleeding, infection, and malignant transformation.9 We describe a case of a tailgut cyst presenting with gluteal swelling and pelvic pain, along with review of relevant literature.
CASE REPORT A 42-year-old female non-diabetic and non-hypertensive came to our hospital with the chief complaints of swelling in the left buttock for 15years and, pain at the time of defecation since 2-3 months. The swelling was small in size approximately 4cm*3cm*3cm which had progressed gradually to the current size of approximately 12cm*10cm*6cm with pain over the swelling aggravating on sitting for long hours relieved on standing or change in posture. There was no history of swelling elsewhere over the body, no history of any discharge from the swelling, no history of insect or animal bite, no history of trauma, no history of weight loss or loss of appetite. No history of fever with chills or rigors. Past history, family history, menstrual and obstetric history were non-contributory on physical examination, a single swelling was felt over the left gluteal region with well-defined margin (Fig A), globular in shape, cystic in consistency, slightly mobile with no fixity to the underlying muscle, Fluctuation test was positive with no evidence of any local signs of inflammation, discharge from the swelling or a visible puncture or dilated veins. There was no evidence of any lymphadenopathy.
Figure A: Clinical photograph of the gluteal swelling Digital rectal examination revealed a soft mass posterior to the rectal wall, compressing the rectum, and was not mobile. Local Ultrasound of the swelling showed a well-defined cystic lesion of 10cm*10cm*10.5cm(577cc) in the subcutaneous plane with a wall thickness of 4mm with no intramuscular extension. FNAC report revealed scattered and clusters of hemosiderophages admixed with RBCs and proteinaceous eosinophilic material suggestive of hematoma. Clinical diagnosis of the sebaceous cyst was made Excision of the cystic mass by a posterior approach (FigB) was done while removing the cyst ruptured with milky mucous material oozing out. The cyst was carefully separated and was found extending below muscle plane reaching the pelvis up to the posterior wall of the rectum without any connection to the rectum The excised specimen were sent for histopathological diagnosis(Fig C) which was retro-rectal cystic hamartoma (tailgut cyst) with no evidence of malignancy. The patient was discharged after 5 days with no postoperative complications. The patient’s postoperative course was uneventful, and, at four months post-surgery, our patient is symptom-free with no evidence of recurrent or residual disease
Figure B: intra operative photograph of cyst being excised.
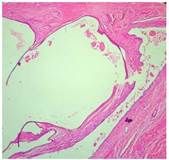
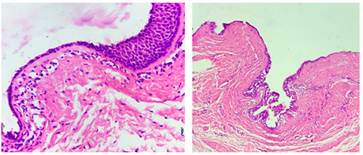
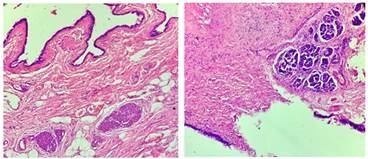
Figure C: Gross image of multilocated cyst Gross examination: We received a cystic mass measuring 8.5x5.0x5.0cm (Fig.C). The cut surface showed multiple cysts (Fig B) and containing mucinous material separated by solid areas with the whitish and dark brown appearance Microscopic examination: Sections showed a multiloculated cyst(Fig E) lined by variable epithelia like respiratory, stratified squamous, cuboidal, and mucin secreting epithelium (Fig F-G). The wall showed mucus glands, glomus bodies (Fig H), islands of pancreatic tissue (Fig I) and smooth muscle bundles. The diagnosis of tailgut cyst was rendered.
Figure E: Microphotograph showing multiloculated cyst (H & E X40)
Figure F Figure G Figure F: Microphotograph showing cyst wall lined by cuboidal to stratified squamous epithelium. (H & E X400); Figure G: Microphotograph of cyst with respiratory and mucinous lining. (H&EX100)
Figure H Figure I Figure H: Microphotograph showing wall of cyst with glomus bodies shown by arrows(H&EX100); Figure I: Microphotograph showing wall of cyst with islands of pancreatic tissue. (H & EX100)
DISCUSSION The retrorectal area is a potential space surrounded by the rectum anteriorly, the sacrum and coccyx posteriorly, and the peritoneal reflection superiorly. A space-occupying lesion, such as a tailgut cyst, in this region, can lead to different symptoms and a variety of clinical signs.10,11 In the process of embryologic development of the tailgut or postanal gut, the embryo has a true tail, which reaches its largest diameter on the 35th day of gestation. Hereafter, the anus develops above the tail on the 56th day of gestation, by which time the latter has completely regressed.8,12 Tailgut cysts is a rare congenital lesion thought to arise from the embryonic postanal gut, well described by Hjermstad et al. in a series of 53 cases.4 They are often lined with mucin-secreting columnar cells, squamous, transitional, or a combination histology.9 Tailgut cysts may also be located in perirenal and subcutaneous areas.8,13 The gluteal region is a rare site and symptoms often depend on the size and relation to the adjacent structures and may even be incidental finding4 Infection is the most frequent complication (occurring in 40-50% of cases). Additionally, tailgut cysts are detected as asymptomatic masses but may be found in patients who present with abdominal pain, rectal bleeding, local abscess, and rectal fullness or constipation.12 There can also be a communication between tailgut cyst and skin; primary infection may progress to post-inflammatory fibrosis if left untreate.9 Diagnosis is done usually by MRI which is a suitable examination for preoperative evaluation of tailgut cyst. MRI improves tissue characterization because of its high contrast resolution between different tissue compartments. It also allows detection of mucin and blood in a cystic lesion.14 Needle biopsy of cystic pre- sacral lesions is not recommended as a diagnostic tool because of the risk of life-threatening infections and it is rarely diagnosed on FNA15 Histopathology gives the final diagnosis The differential diagnosis of tailgut cysts includes sacrococcygeal teratoma, epidermoid cyst, rectal duplication cyst.17 In the differential diagnosis of presacral masses, the unilocular or multilocular characteristic is important. Tailgut cyst and lymphangioma are usually multicystic. MR imaging may be useful for the differentiation of unilocular and multilocular masses.18 A tailgut cyst can transform into a tumor in 2-13% such as an adenocarcinoma, carcinoid, neuroendocrine carcinoma, or sarcoma.12 Hjermstad and Helwig4 reported on one case (2%) of poorly differentiated carcinoma in a series of 53 tailgut cysts. Prasad et al. reported on two cases (40%) of malignancy in a series of five tailgut cysts. Therefore, tailgut cyst need complete surgical excision to prevent (and treat) complications, such as infection, recurrence, and malignant transformation.16 When a tailgut cyst is diagnosed, surgical excision is necessary because of the undesired, life-threatening complications in long-standing cases.15 The surgical approach depends on the location within the presacral space, the size of the lesion, and the presence of complications. For most tailgut cysts, a posterior approach with or without excision of the coccyx bone will allow a good surgical view and removal of the multiloculated cyst.4 For high lesions that occupy most of the presacral space, a trans-abdominal approach is usually required for treatment. For the treatment of large external tumors, a combined approach may be required.3 In summary, tailgut cysts are rare congenital lesions originating from a remnant of the embryonic postanal gut tailgut. They often occur in the presacral retrorectal space, rarely can present as a gluteal mass These cystic lesions should undergo definitive resection because of the risk of malignant transformation. Hence awareness of this entity is essential for correct diagnosis and proper management of presacral lesions.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home